Patient Information

The mission
Choosing Wisely Canada is a campaign to help physicians and patients engage in conversations about unnecessary tests, treatments and procedures, and to help physicians and patients make smart and effective choices to ensure high-quality care.
62% of Canadians agree that there is a significant amount of unnecessary care in the health care system.
To date, 45 different medical and surgical specialties have joined the Choosing Wisely Canada campaign, representing over 90% of physicians in Canada. Societies representing these specialties have developed evidence-based lists of “top 5” tests and treatments for which there is strong evidence of overuse, waste, or even possible harm to patients.
92% of Canadians believe patients need more support to know which services are really necessary for their health.
Over 150 physician recommendations have been released across this wide spectrum of specialties. Over 25 corresponding lay language patient materials have also been released to help facilitate the conversation with patients.
68% of Canadian family physicians agree that more tools are needed to help them make decisions about which services are inappropriate for their patients.
For more information on Choosing Wisely Canada, and to view all physician recommendations and patient materials, please visit our website, ChoosingWiselyCanada.org. To browse our recommendations and patient materials with ease, download our mobile app by searching for “Choosing Wisely Canada” in your Apple App or Google Play store.
More is not always better philosophy & approach
Since the launch of Choosing Wisely Canada in April 2014, significant effort has gone into educating physicians and mobilizing the health care provider community to adopt the published recommendations. And these efforts are beginning to pay off as impressive results are beginning to emerge across different clinical settings across Canada.
However, these provider-driven efforts are not enough. There is evidence suggesting that patients also play an important role in driving unnecessary care. In fact, in a recent survey of Canadians conducted by Ipsos Reid for Choosing Wisely Canada, 67% of respondents said that “patient demands are responsible for more unnecessary use of health services than are decisions by physicians”. Clearly, the perception that “more is better” needs to be addressed.
The More Is Not Always Better campaign will do the following:
- Promote the message that in medicine as it is in life, “more is not always better”.
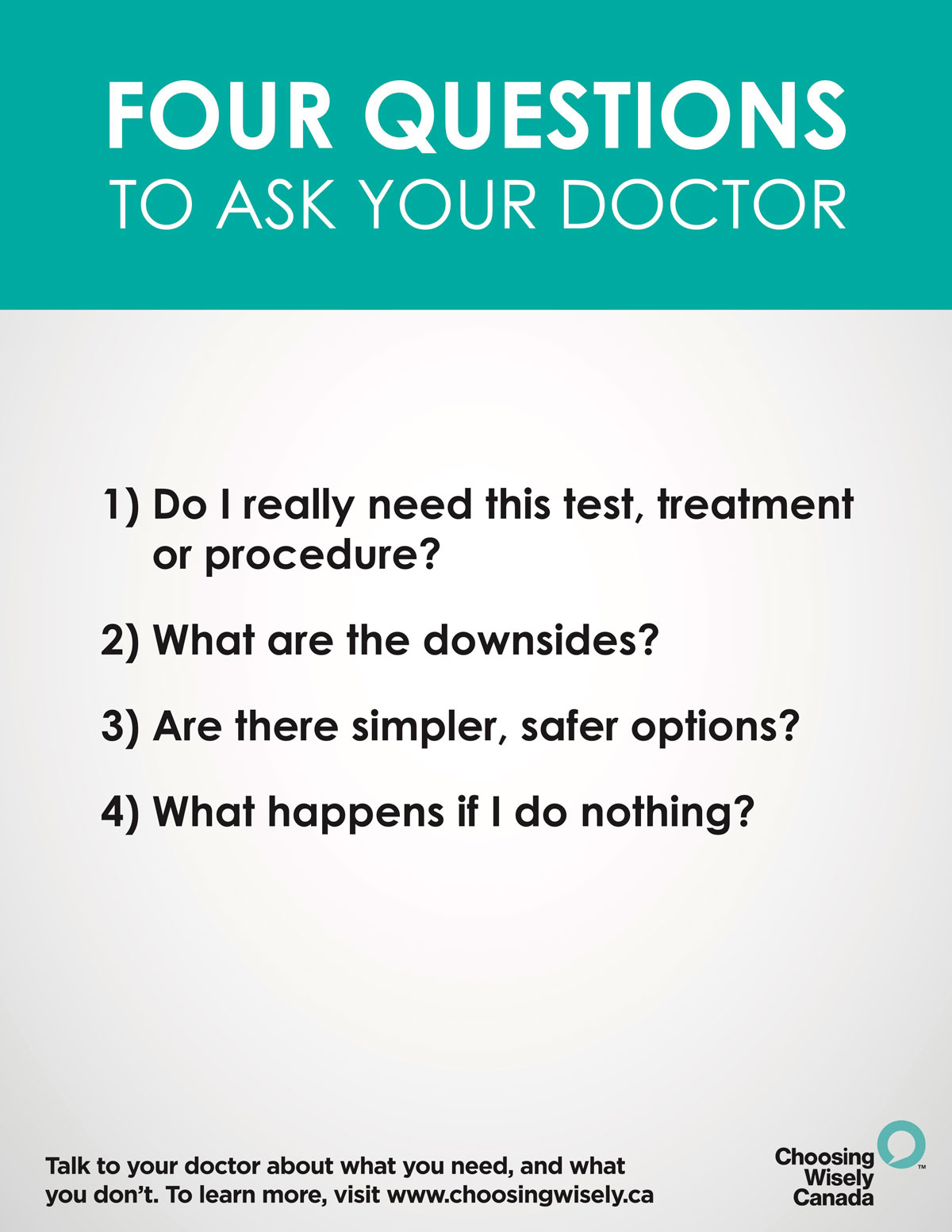
- Educate patients about when they might need a particular test or treatment, and when they don’t.
- Encourage patients to talk with their doctor about unnecessary care.
Eleven things Physicians and Patients should question
Don’t do imaging for lower-back pain unless red flags are present.
Red flags include, but are not limited to, severe or progressive neurological deficits or when serious underlying conditions such as osteomyelitis are suspected. Imaging of the lower spine before six weeks does not improve outcomes.
Don’t use antibiotics for upper respiratory infections that are likely viral in origin, such as influenza-like illness, or self-limiting, such as sinus infections of less than seven days of duration.
Bacterial infections of the respiratory tract, when they do occur, are generally a secondary problem caused by complications from viral infections such as influenza. While it is often difficult to distinguish bacterial from viral sinusitis, nearly all cases are viral. Though cases of bacterial sinusitis can benefit from antibiotics, evidence of such cases does not typically surface until after at least seven days of illness. Not only are antibiotics rarely indicated for upper respiratory illnesses, but some patients experience adverse effects from such medications.
Don’t order screening chest X-rays and ECGs for asymptomatic or low risk outpatients.
There is little evidence that detection of coronary artery stenosis in asymptomatic patients at low risk for coronary heart disease improves health outcomes. False positive tests are likely to lead to harm through unnecessary invasive procedures, over-treatment and misdiagnosis. Chest X-rays for asymptomatic patients with no specific indications for the imaging have a trivial diagnostic yield, but a significant number of false positive reports. Potential harms of such routine screening exceed the potential benefit.
Don’t screen women with Pap smears if under 21 years of age or over 69 years of age.
- Don’t do screening Pap smears annually in women with previously normal results
- Don’t do Pap smears in women who have had a hysterectomy for non-malignant disease
The potential harm from screening women younger than 21 years of age outweighs the benefits and there is little evidence to suggest the necessity of conducting this test annually when previous test results were normal. Women who have had a full hysterectomy for benign disorders no longer require this screening. Screening should stop at age 70 if three previous test results were normal.
Don’t do annual screening blood tests unless directly indicated by the risk profile of the patient.
There is little evidence to indicate there is value in routine blood tests in asymptomatic patients; instead, this practice is more likely to produce false positive results that may lead to additional unnecessary testing. The decision to perform screening tests, and the selection of which tests to perform, should be done with careful consideration of the patient’s age, sex and any possible risk factors.
Don’t routinely measure Vitamin D in low risk adults.
Because Canada is located above the 35° North latitude, the average Canadian’s exposure to sunlight is insufficient to maintain adequate Vitamin D levels, especially during the winter. Therefore, measuring serum 25-hydroxyvitamin D levels is not necessary because routine supplementation with Vitamin D is appropriate for the general population. An exception is made for measuring Vitamin D levels in patients with significant renal or metabolic disease.
Don’t routinely do screening mammography for average risk women aged 40 - 49.
If, after careful assessment of women less than 50 years of age, their risk profile for breast cancer is low, the benefit of screening mammography is also quite low. Furthermore, for this age group there is a greater risk of a false-positive and consequently undergoing unnecessary or harmful follow-up procedures.
Don’t do annual physical exams on asymptomatic adults with no significant risk factors.
A periodic physical examination has tremendous benefits; it allows physicians to check on their healthy patients while they remain healthy. However, the benefits of this check-up being done on an annual basis are questionable since many chronic illnesses that benefit from early detection take longer than a year to develop. Preventive health checks should instead be done at time intervals recommended by guidelines, such as those noted by the Canadian Task Force on the Periodic Health Examination.
Don’t order DEXA (Dual-Energy X-ray Absorptiometry) screening for osteoporosis on low risk patients.
While all patients aged 50 years and older should be evaluated for risk factors for osteoporosis using tools such as the osteoporosis self-assessment screening tool (OST), bone mineral density screening via DEXA is not warranted on women under 65 or men under 70 at low risk.
Don’t advise non-insulin requiring diabetics to routinely self-monitor blood sugars between office visits.
While self-monitoring of blood glucose (SMBG) for patients with diabetes is recommended by certain groups to help monitor glycemic control, for most adults with type II diabetes who are not using insulin, many studies have shown that routine SMBG does little to control blood sugar over time.
Don’t order thyroid function tests in asymptomatic patients.
The primary rationale for screening asymptomatic patients is that the resulting treatment results in improved health outcomes when compared with patients who are not screened. There is insufficient evidence available indicating that screening for thyroid diseases will have these results.